Heart Failure And Covid
People with a pre-existing heart problem like heart failure are about 10% to 20% more likely to experience severe illness from COVID-19 compared to people with healthy hearts. They are also more likely to get much sicker and even die because of COVID-19.
Research has shown that people who have a history of heart failure who are hospitalized for COVID-19 are nearly twice as likely to die than those who dont. COVID-19 patients with heart failure had hospital stays averaging about two days longer than those without the condition, and they were twice as likely to require mechanical ventilation.
Heart Failure Treatments And Covid
The key to managing heart failure is adhering to a treatment strategy that includes medications and lifestyle changes. In severe cases, implants or surgeries may be required. Some common prescription medications used to treat heart failure include:
- Angiotensin-converting enzyme inhibitors like captopril, lisinopril, enalapril, and ramipril
- Angiotensin receptor blockers like valsartan and losartan
- Beta-blockers like carvedilol, metoprolol succinate, and bisoprolol
- Angiotensin receptor neprilysin inhibitor
- Diuretics like furosemide and torsemide
- SGLT2 inhibitors like empagliflozin
Many of these medications carry a risk of side effects like dizziness, low blood pressure, shortness of breath, and difficulty breathing. These symptoms can be exacerbated by COVID-19 or make a coronavirus infection feel worse.
People with heart failure should stick to the medication regimen prescribed by their healthcare providereven if they have COVID-19. Call your practitioner before making any medication changes on your own.
Inclusion And Exclusion Criteria
We identified all patients who had a VA hospital stay during fiscal years 20022007 with a prior diagnosis of COPD , ninth revision codes 490492 or 496) and a primary discharge diagnosis of pneumonia or a secondary discharge diagnosis of pneumonia with a primary diagnosis of respiratory failure or sepsis .
We included elderly patients in this study if they 1) were aged 65 years on the date of hospital presentation 2) had 1 year of VA outpatient care before admission 3) had received at least one of the following respiratory medications during the 30-day period before hospitalisation: any form of -agonist, theophylline, tiotropium or ipratropium bromide and 4) had received at least one dose of antibiotics within 48 h of admission. For patients with multiple hospitalisations, we only assessed the first admission during the study period.
We excluded patients with history of asthma .
Recommended Reading: Congestive Heart Failure Prevention
This Symptom Is Often Misdiagnosed As A Respiratory Problem
Most commonly, a cough that wont quit is the result of asthma or chronic obstructive pulmonary disease . However, as the Cleveland Clinic points out, even with these diseases, coughing is minimized when inflammation in the lungs is kept under control.
Their experts say that if your cough persists after treatmenteven if youve been diagnosed with a respiratory ailmentyou should be evaluated for heart failure. I have met patients who were first diagnosed as having a respiratory issue, heart failure specialist Miriam Jacob, MD, explains via the Cleveland Clinic site. Over time, when their symptoms did not improve with appropriate treatment, heart failure was entertained as a diagnosis.
Recommended Reading: What Is Normal Heart Rate When Exercising
Can You Survive Pneumonia With Heart Failure
For patients with heart failure, the risk of dying after an episode of pneumonia is up to fourfold higher than if they had not contracted the disease, with the risk for vascular events and death remaining high for months after recovery, according to a post hoc analysis of the PARADIGM-HF and PARAGON-HF trials.
How does pneumonia affect congestive heart failure?
An acute infection like pneumonia increases the stress on the heart and can lead to a cardiac event like heart failure, heart attack or arrhythmias, said Weston Harkness, DO, a cardiology fellow at Samaritan Cardiology Corvallis. For a healthy person, a case of pneumonia is very unlikely to lead to a cardiac event.
Recommended Reading: Homemade Dog Food For Congestive Heart Failure
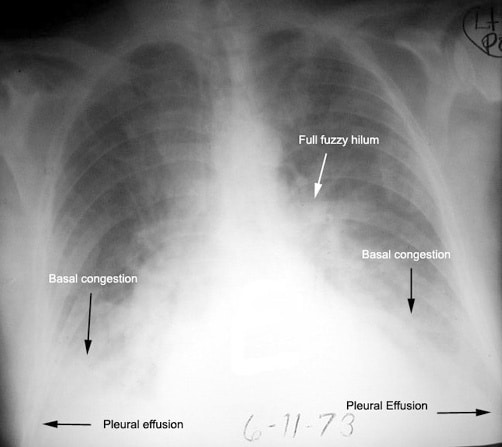
What Procedures And Tests Diagnose Congestive Heart Failure
Congestive heart failure can be a medical emergency, especially if it acutely decompensates and the patient can present extremely ill with the inability to breathe adequately. In this situation, the ABCs of resuscitation need to be addressed while at the same time, the diagnosis of congestive heart failure is made.
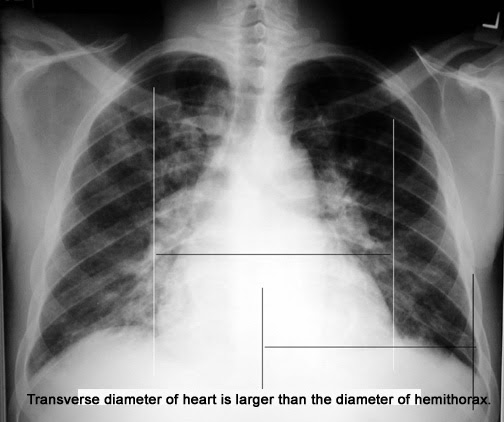
Common tests that are done to help with the diagnosis of congestive heart failure include the following:
- Electrocardiogram to help assess heart rate, rhythm, and indirectly, the size of the ventricles and blood flow to the heart muscle.
- Blood tests may include a complete blood count , electrolytes, glucose, BUN, and creatinine .
- B-type natriuretic peptide may be helpful in deciding if a patient has shortness of breath from congestive heart failure or from a different cause. It is a chemical that is located in the heart ventricles and may be released when these muscles are overloaded.
- Echocardiography or ultrasound testing of the heart is often recommended to assess the anatomy and the function of the heart. In addition to being able to evaluate the heart valves and muscle, the test can look at blood flow within the heart, watch the chambers of the heart contract, and measure the ejection fraction .
Other tests may be considered to evaluate and monitor a patient with suspected congestive heart failure, depending upon the clinical situation.
Most symptoms caused by heart failure can be divided into three general categories:
An Inflammatory Response: Cardiovascular Complications Of Pneumonia
Each year, community-acquired pneumonia affects an estimated 5 to 6 million Americans and leads to 60,000 deaths.1 In addition to its respiratory effects, CAP and other acute infections can cause or exacerbate cardiovascular complications through various mechanisms. A systematic review and meta-analysis published in 2011 reported that 18% of patients with CAP developed CV complications within 30 days of CAP diagnosis, with higher rates found in hospitalized patients compared with outpatients.2
The strongest risk factor for CV complications in patients with pneumonia is pre-existing CVD, which is present in more than half of elderly patients hospitalized for CAP.3,4 The risk of developing CAP is up to 3 times greater in individuals with chronic CVD, especially heart failure, and those individuals with cerebrovascular disease have twice the risk for CAP.5
Although the precise mechanisms by which CAP may trigger CV complications have not been identified, it has been proposed that many CV complications result from the interactions between demographic characteristics of the patients , pneumonia severity and host reactions to the infection of the lower respiratory tract, wrote the authors of a recent review published in Respirology.2,6Once pneumonia is established, the host remains in a relative hypoxaemic state secondary to alveolar consolidation that affects the normal ventilation/perfusionhomeostasis.
Arrhythmias
Recommended Reading: What Is Good Heart Rate Recovery
What Is Congestive Heart Failure
Heart failure describes the inability or failure of the heart to meet the needs of organs and tissues for oxygen and nutrients. This decrease in cardiac output, the amount of blood that the heart pumps, is not adequate to circulate the blood returning to the heart from the body and lungs, causing the fluid to leak from capillary blood vessels. This leads to symptoms that may include shortness of breath, weakness, and swelling.
Understanding blood flow in the heart and body
The right side of the heart pumps blood to the lungs while the left side pumps blood to the rest of the body. Blood from the body enters the right atrium through the vena cava. It then flows into the right ventricle where it is pumped to the lungs through the pulmonary artery, which carries deoxygenated blood to the lungs. In the lungs, oxygen is loaded onto red blood cells and returns to the left atrium of the heart via the pulmonary veins. Blood then flows into the left ventricle where it is pumped to the organs and tissues of the body. Oxygen is downloaded from red blood cells into the various organs while carbon dioxide, a waste product of metabolism, is added to be removed in the lungs. Blood then returns to the right atrium to start the cycle again. The pulmonary veins are unusual in that they carry oxygenated blood, while the pulmonary artery carries deoxygenated blood. This is a reversal of duties versus the roles of veins and arteries in the rest of the body.
The Impact Of Cough On Heart Function
Cough influences heart function either by its effects on intrathoracic pressure resulting in cardiovascular hemodynamic consequences or by influencing heart electrophysiology causing an arrhythmogenic effect. It is difficult to distinguish or separate these two phenomena due to their interplay .
Possible impact of cough on heart function
The impact of cough on the cardiovascular system has been documented in numerous previous studies, especially in the context of cough-induced arrhythmias, cough-induced conduction disorders or cough-induced syncope. However, controversies still exist on the role of cough in cardiopulmonary resuscitation. These conditions will be discussed below.
Read Also: Why Do Soccer Players Have Heart Attacks
Strengths And Limitations Of Study
The putative role of community acquired pneumonia on heart failure, and cardiac disease in general, is still evolving. Pneumonia increases systematic oxidative stress and inflammatory markers , in both the short term and the long term, leading to an increased risk of thrombogenesis, destabilisation of atherosclerotic plaques, and endothelial dysfunction, potentially leading to increased rates of ischaemic heart disease, atrial fibrillation, and reduced ventricular function.61637 Furthermore, this increased host response to infection has been shown to occur even in those with less severe infections and to persistent long after a patient clinically recovers from the acute infection.31 Whether community acquired pneumonia truly causes heart failure in itself or whether heart failure is simply the endgame in the cardiac cascade triggered by acute pneumonia event is not fully elucidated. Other factors, which are common to both pneumonia and heart failure, are also likely at play, including advanced age, reduced renal function, and the presence of other major comorbidities , and collectively are likely to contribute to the increased risk of heart failure in patients with pneumonia.6 A major limitation of our study is that we could not examine these potential mechanisms and causes of heart failure related to pneumonia.
Why Its Important To Know Your Ef
If you have a heart condition, it is important for you and your doctor to know your EF. Your EF can help your doctor determine the best course of treatment for you. Measuring your EF also helps your healthcare team check how well our treatment is working.
Ask your doctor how often you should have your EF checked. In general, you should have your EF measured when you are first diagnosed with a heart condition, and as needed when your condition changes.
Also Check: How Do I Cure Pneumonia
You May Like: Post Open Heart Surgery
Pneumonia Risk Soars In Heart Failure Patients Especially Hfpef
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Patients with heart failure get pneumonia at a rate almost three times greater than expected and, once they do get pneumonia, have about a fourfold greater risk of death, investigators for a retrospective analysis of 13,000 patients from two landmark randomized HF trials have found.
Dr. John J.V. McMurray
The investigators also found that HF patients with preserved ejection fraction are at the highest risk of developing pneumonia. The findings underscore the importance of patients with HF getting a pneumonia vaccination, they found.
The analysis showed that 6.3% of patients in the PARADIGM-HF trial and 10.6% of those in the PARAGON-HF trial developed pneumonia, reported the study authors, led by John J.V. McMurray, MD, of the British Heart Foundation Cardiovascular Research Center at the University of Glasgow in Scotland .
The main reason for doing this study was the fact that many heart failure patients are not vaccinated, as they should be, against pneumonia both pneumococcus and influenza vaccination, Dr. McMurray said in an interview. We wanted to document the frequency and consequences of pneumonia in patients with heart failure to help highlight this deficiency in care.
Dr. McMurray said he believes this is the first study to document the incidence of pneumonia and pneumonia-related outcomes according to the two major ejection fraction phenotypes.
Recommended Reading: Swollen Ankles Heart Failure
Treatment For Pneumonia In A Heart Failure Patient: What To Expect
An elderly person with pneumonia, who has pre-existing heart failure, presents a tricky situation to doctors.
My very elderly father, who has congestive heart failure, was diagnosed with pneumonia at an urgent care center. The doctor wanted him admitted to a hospital.
When my mother was diagnosed with pneumonia for the first time at an elderly age, she too, had congestive heart failure, but was not admitted, and instead, sent home with a prescription for antibiotics and recovered.
A few years later she developed pneumonia a second time and was admitted overnight in the observation unit, but discharged the next day with a prescription for antibiotics and recovered.
I anticipated that my father, whose heart was seemingly stronger than my mothers, would be discharged the next day with a prescription for antibiotics.
But he was discharged from the hospital seven days later.
Heres a summary of how the pneumonia treatment went down, due to the pre-existing heart failure.
The pneumonia treatment involved an IV infusion of fluids. Due to the pre-existing heart failure, my father was on Lasix, a diuretic that promotes fluid excrement from the body.
Early on in his admission, my fathers weight went up, which meant unwanted fluid retention.
It was not clear exactly how much of this was being caused by the IV infusion of fluids any fluid buildup in the lungs from the pneumonia or the pre-existing heart failure being worsened by the infection.
Peripheral edema. Shutterstock/AppleDK
You May Like: What To Take For Heart Attack
What Is The Connection Between Congestive Heart Failure
Congestive heart failure often leads to pneumonia because it leads to buildup of fluids in the lung. The build up can result in infection which can then cause pneumonia if its not treated quickly. My grandfather experienced this. He had congestive heart disease and then, he also developed pneumonia. He was in the hospital for a long time.
Complications Of Heart Failure And Covid
People with heart failure are at a greater risk of becoming severely ill with COVID-19. One study found that among patients who were hospitalized with a COVID-19 infection, there was a 50% mortality rate among those with pre-existing heart failure compared with a mortality rate of 10% in individuals without heart failure.
Treatment for COVID-19 can also lead to serious complications for people with heart failure due to several contributing factors:
- Breathing can be difficult for people with heart failure even without a COVID-19 infection. Fluid can accumulate in the body, particularly in the lungs, since blood that cant be pumped throughout the body causes a backup. This can further reduce the much-needed oxygen supply in people with heart failure. Additionally, COVID-19 usually results in pneumonia and decreased movement of oxygen across the cells in the lung to the bloodstream.
- As COVID-19 and heart failure create difficulty for the body to breathe and pump blood, a persons chances of requiring mechanical ventilation increase. This may seem like the fix. However, especially for people with heart failure, there has been evidence that the high pressure required to support the breathing of people with COVID-19 on mechanical ventilation can further increase pressure in the pulmonary vessels. This creates even greater strainand damageto the heart.
- Severe COVID-19 infection has also been known to cause kidney damage, which can further increase the workload of the heart.
You May Like: Sings Of Heart Attack In Women
Outcomes Of Pneumonia In Patients With Heart Failure
- Shen L, Jhund PS, Anand IS, et al.
- Citation:
- Supriya Shore, MD
Quick Takes
- In post hoc analyses of two large, randomized cohorts with HFrEF and HFpEF patients, incidence of pneumonia was 29 and 39 per 1,000 patient-years, respectively.
- Patients with pneumonia in both cohorts were older with more comorbid conditions.
- Pneumonia was associated with an increased risk of two- to four-fold for HF hospitalization, all-cause mortality, and cardiovascular mortality in both HFrEF and HFpEF patients.
How Do You Stop Coughing With Congestive Heart Failure
There are a few things that can be done to stop coughing with congestive heart failure. One is to take medications prescribed by a doctor to help loosen secretions and make it easier to cough up phlegm. Another is to drink plenty of fluids, which will help thin out mucus. And finally, practicing good hygiene by regularly washing hands and avoiding contact with respiratory viruses can help reduce the risk of infection.
You May Like: Can Dehydration Cause Low Heart Rate
Also Check: Can Ekg Detect Heart Failure
Comparison With Other Studies
Our study also builds on the evidence for patients with pneumonia managed as outpatients. Only one previous study has evaluated the impact of pneumonia on heart failure in patients managed on an outpatient basis. In 907 outpatients, the Pneumonia Patient Outcomes Research Team observed an incident rate of heart failure of 1.4% within 30 days.11 Conversely, within 90 days only 0.9% of outpatients had incident heart failure in our study . Again, the PORT study was fairly restrictive in the spectrum of patients included in their study and, unlike our study, was not population based.
Risk Of Heart Failure After Community Acquired Pneumonia: Prospective Controlled Study With 10 Years Of Follow
- Accepted 11 January 2017
You May Like: Best Way To Prevent Heart Attack
