How Can I Reduce The Extra Fluid In My Body
Cardiologists and registered dietitians can help you manage fluid retention with medicine and nutrition plans. Here are a few steps you can take at home.
- Monitor your weight and lose weight if needed Talk with your doctor about what your ideal weight is. Your “dry weight” is your regular weight when you are not retaining fluid.
- Cut back on salt/sodium Salt is the main source of sodium, which is found naturally in and also added to many of the foods we eat. Sodium causes your body to hold on to water. Most nutrition plans for CHF patients limit sodium to 1500 to 2,000 milligrams or less per day.
- Take diuretics as directed Diuretics, also known as water pills, help your kidneys remove extra water and salt from your body. They can also relieve swelling in your legs.
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Get Rid Of The Salt Shaker
When it comes to reducing salt in your diet, out of sight, out of mind is an effective approach. Simply getting rid of the salt shaker in your kitchen or on the dinner table can make a big impact.
Need some motivation? One shake of salt contains about 250 mg of sodium, which is one-eighth of your daily intake.
Don’t Miss: How Does Blood Flow Through The Heart
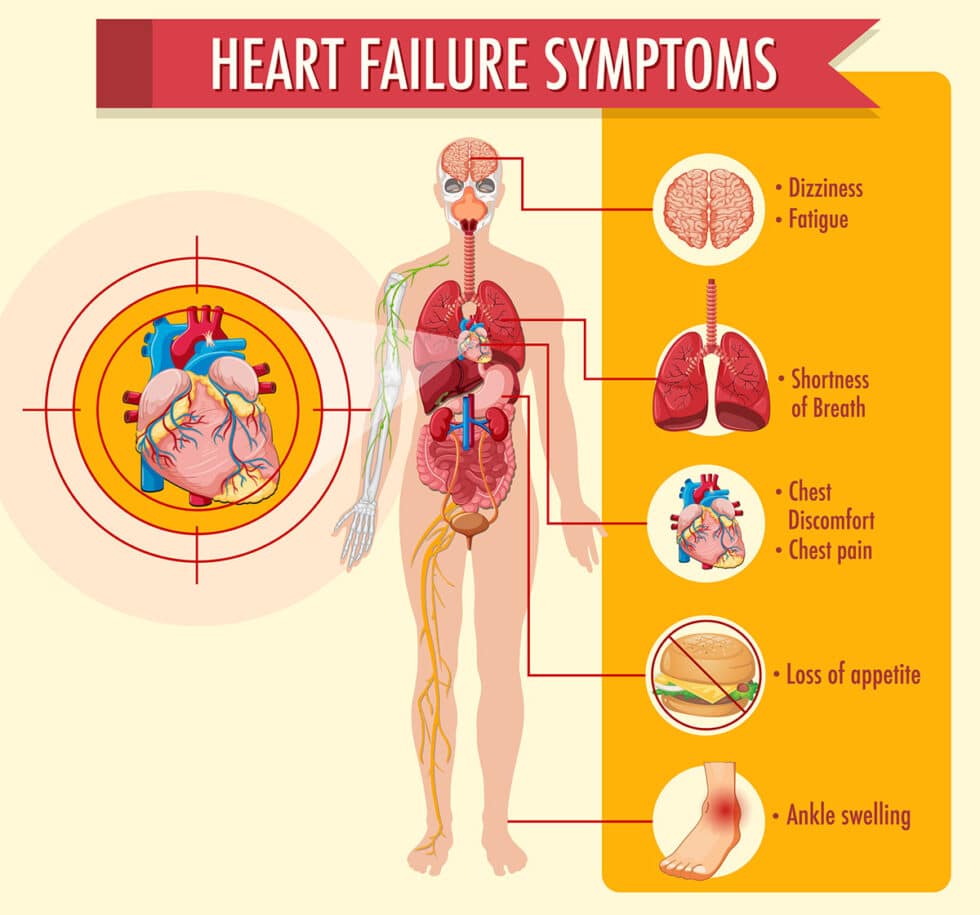
What Are The Symptoms Of Heart Failure
You may not have any symptoms of heart failure, or the symptoms may be mild to severe. Symptoms can be constant or can come and go. The symptoms can include:
- Congested lungs. Fluid backup in the lungs can cause shortness of breath with exercise or difficulty breathing at rest or when lying flat in bed. Lung congestion can also cause a dry, hacking cough or wheezing.
- Fluid and water retention. Less blood to your kidneys causes fluid and water retention, resulting in swollen ankles, legs, abdomen , and weight gain. Symptoms may cause an increased need to urinate during the night. Bloating in your stomach may cause a loss of appetite or nausea.
- Dizziness, fatigue, and weakness. Less blood to your major organs and muscles makes you feel tired and weak. Less blood to the brain can cause dizziness or confusion.
- Rapid or irregular heartbeats. The heart beats faster to pump enough blood to the body. This can cause a rapid or irregular heartbeat.
If you have heart failure, you may have one or all of these symptoms or you may have none of them. They may or may not indicate a weakened heart.
Initial Stages Of Chf
In the initial, mild stage A, there are underlying high-risk factors for CHF such as smoking or high blood pressure. However, the affected person has no symptoms or limitations at rest or with physical activity and there are no signs of CHF on evaluation by a doctor.
In stage B, the person develops mild symptoms of fatigue, shortness of breath, or heart palpitations with routine physical activity. There are minor signs of heart dysfunction on a doctor’s evaluation. There might also be a mild, intermittent collection of fluid, known as edema, in the ankles and feet.
Read Also: What Is A Normal Heart Rate For A Pregnant Woman
Prognosis At Different Ages
In general, younger people diagnosed with CHF tend to have a better outlook than older people.
A report averaging several smaller studies found that people under age 65 generally had a 5-year survival rate of 78.8 percent following CHF diagnosis. The same report found that people over age 75 had an average 5-year survival rate of 49.5 percent following diagnosis.
Older people diagnosed with CHF may already have other chronic health conditions. This can make it difficult to manage CHF and create a more challenging outlook for them.
for congestive heart failure. The treatment thats best for you will depend on:
- your overall health
- any other health conditions you have
- how you respond to any medications
- what stage of CHF you have
Common options include:
There are lifestyle changes a person with CHF can make that have been shown to help slow the conditions progression. Talk with your doctor before making changes to your diet or starting an exercise routine.
What Medications Should I Avoid If I Have Heart Failure
There are several different types of medications that are best avoided in those with heart failure including:
- Nonsteroidal anti-inflammatory medications such as Motrin or Aleve. For relief of aches, pains, or fever take Tylenol instead.
- Most calcium channel blockers
- Some nutritional supplements, such as salt substitutes, and growth hormone therapies
- Antacids that contain sodium
If youâre taking any of these drugs, discuss them with your doctor.
Itâs important to know the names of your medications, what theyâre used for, and how often and at what times you take them. Keep a list of your medications and bring them with you to each of your doctor visits. Never stop taking your medications without discussing it with your doctor. Even if you have no symptoms, your medications decrease the work of your heart so that it can pump more effectively.
Read Also: Emergency Open Heart Surgery
What Are The Types Of Heart Failure
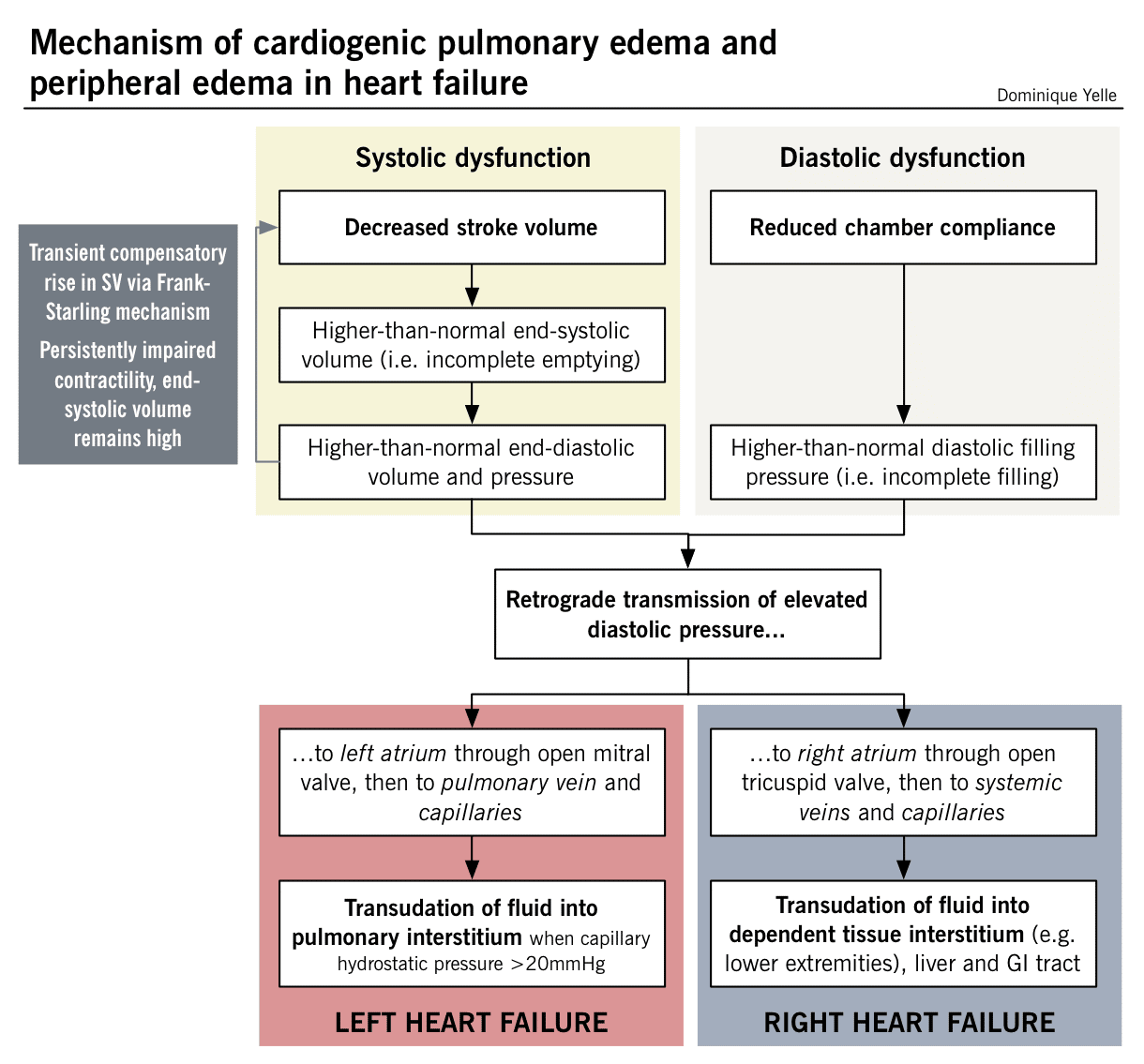
Systolic dysfunction happens when the heart muscle doesn’t contract with enough force, so there is less oxygen-rich blood pumped throughout the body.
Diastolic dysfunction happens when the heart contracts normally, but the ventricles donât relax properly or are stiff, and less blood enters the heart during normal filling.
A calculation done during an echocardiogram, called the ejection fraction , is used to measure how well your heart pumps with each beat to help determine if systolic or diastolic dysfunction is present. Your doctor can discuss which condition you have.
How Does Heart Failure Affect The Quality Of Life And Lifestyle
With the right care and treatment plan, many adults still enjoy life even though heart failure limits their activities. How well you feel depends on:
- How well your heart muscle is working.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
This includes caring for yourself by:
- Taking your medications.
Don’t Miss: Stroke After Open Heart Surgery
Moderate Stage Of Chf
At Stage C, as the heart continues to fail, the person develops weakness and significant fatigue, shortness of breath or palpitations with the slightest physical exertion. She begins to limit activity because of these symptoms as she is only comfortable when resting. A doctor’s evaluation and testing shows moderate signs of heart dysfunction,
Other possible symptoms might include more visible edema of the lower extremities and the hands might also swell as the fluid congestion in body tissues increases. Shoes and rings might be tighter. The pulse might become weaker because of the struggling heart.
Find Alternative Thirst Quenchers
Its tempting to guzzle a bunch of water when youre thirsty. But sometimes, just moistening your mouth can do the trick.
The next time youre tempted to gulp down some water, try these alternatives.
- Swish water around your mouth and spit it out.
- Suck on sugar-free candy or chew sugar-free gum.
- Roll a small ice cube around the inside of your mouth.
Also Check: Can Gas Cause Heart Palpitations
Why Does Heart Failure Cause Edema
Although it sounds like the heart is failing to work at all, the term heart failure really means that the heart has grown weaker or stiffer. It still pumps blood, but its not enough to meet the bodys needs.
Heart failure can result from several issues, including:
- various types of heart disease
Diseases like diabetes and sleep apnea can also weaken the heart.
Since the heart isnt able to adequately pump blood out through the arteries and bring it back through the veins, blood can begin to pool, especially in the legs and feet.
The veins require a certain amount of force from the heart to keep blood flowing up to the heart and lungs, where it receives oxygen and other nutrients. The pressure inside the veins is also higher due to higher pressures in those with heart failure.
Without medications or devices to improve the heart muscles strength, blood doesnt circulate properly in someone with heart failure. Excess blood and other fluids in the capillaries can leak out into bodily tissues, causing edema.
Sometimes edema is the first sign of heart failure. Once heart failure is diagnosed, it becomes important to monitor increases in body weight that may result from increased fluid retention.
There are three main types of heart failure. Each one reduces the hearts ability to pump effectively.
When To Call The Doctor

- You are tired or weak.
- You feel short of breath when you are active or when you are at rest.
- You feel short of breath when you lie down, or an hour or two after falling asleep.
- You are wheezing and having trouble breathing.
- You have a cough that does not go away. It may be dry and hacking, or it may sound wet and bring up pink, foamy spit.
- You have swelling in your feet, ankles, or legs.
- You have to urinate a lot, particularly at night.
- You have gained or lost weight.
- You have pain and tenderness in your belly.
- You have symptoms that you think might be from your medicines.
- Your pulse, or heartbeat, gets very slow or very fast, or it is not steady.
Also Check: Heart Failure And Blood Pressure
Effects Of Fluid Retention
As fluid settles in different areas of the body, seniors may experience a range of symptoms.
- The fluids can settle in the lungs or chest cavity, resulting in shortness of breath or cough.
- If fluids settle in the extremities, individuals may experience swelling and weight gain due to fluid retention.
- Seniors may also experience bloating in their stomachs as fluid settles in the abdomen, reducing their appetite or causing nausea.
If a senior notices sudden swelling or changes in symptoms, they should seek medical attention immediately. The symptoms of CHF and fluid buildup as a result of the condition are gradual, so any sudden change is a sign that something else could be going on.
RELATED CONTENT: The Importance of Home Care for Seniors with CHF
Can You Prevent Congestive Heart Failure
Congestive heart failure can be the ultimate result of a number of diseases, or lifestyle choices, that damage the heart. Some of these can be prevented. Others cannot be prevented but can be treated successfully.
Some examples of illnesses or lifestyle choices that can lead to congestive heart failure are as follows:
- Damage to the heart valves
In some cases, a family history of heart failure can be present. Many cases are a combination of factors, and in other cases, the cause is unknown.
If a person has congestive heart failure, they are at increased risk of developing pneumonia. They probably should receive both the pneumonia vaccination and annual flu shots. Patients should ask their doctor or other health care professional to be sure.
Recommended Reading: Can You Have Afib With Normal Heart Rate
What Are Heart Failure Symptoms
If you have heart failure, you may not have any symptoms, or the symptoms may range from mild to severe. Symptoms can be constant or can come and go. Heart failure symptoms are related to the changes that occur to your heart and body, and the severity depends on how weak your heart is. The symptoms can include:
- Congested lungs. A weak heart causes fluid to back up in the lungs. This can cause shortness of breath with exercise or difficulty breathing at rest or when lying flat in bed. Lung congestion can also cause a dry, hacking cough or wheezing.
- Fluid and water retention. A weak heart pumps less blood to your kidneys and causes fluid and water retention, resulting in swollen ankles, legs, and abdomen and weight gain. This can also cause an increased need to urinate during the night as your body attempts to get rid of this excess fluid. Bloating in your stomach may cause a loss of appetite or nausea.
- Dizziness, fatigue, andweakness. Less blood to your major organs and muscles makes you feel tired and weak. Less blood to the brain can cause dizziness or confusion.
- Rapid or irregular heartbeats. The heart beats faster to pump enough blood to the body. This can cause a fast or irregular heartbeat. Irregular heartbeats also can become more common as the heart weakens.
Diuretic Resistance And Crs Syndrome
Several studies that used different metrics tried to establish a correlation between efficacy of diuretics and heart failure-related clinical outcomes. In the case of patients having reduced diuretic efficacy, Testani et al. found high mortality rates even after correcting for diuretic dose and fluid output. Valente et al. and Voors et al. observed increased death and rehospitalization rates associated with diuretic resistance in heart failure at 60 days, whereas Ter Maaten et al. reported similar outcomes at 30-day follow-up. After correcting for the GFR, Verbrugge et al. and Singh et al. reported higher death and rehospitalization rates related to diuretic resistance.
Acute CRS is a reflection of worsening renal function in patients with CHF . CRS is found in 2533% of all patients with acute decompensated heart failure . Extrarenal hemodynamic changes, cellular dysregulation, neurohormonal activation, and intrarenal microvascular and oxidative stress underlie acute CRS . In a few cases, intravenous diuretic-mediated renal injury is responsible for worsening renal function . Other proposed mechanisms of CRS pathophysiology include neurohumoral adaptations, reduced renal perfusions, elevated venous pressure, and dysfunction of the right ventricle .
Also Check: What Side Of Chest Is Heart On
Read Also: How To Lower Your Heart Rate While Running
Whats The Connection With Congestive Heart Failure
When someone experiences heart failure, one or both of the hearts lower chambers lose the ability to pump blood effectively. The blood can then back up in the legs, ankles, and feet, which leads to swelling, or edema.
If the person spends a lot of time on their back, the swelling can end up in the back.
Heart failure can also cause swelling in the abdomen and sometimes can lead to fluid buildup in the lungs, called pulmonary edema. Pulmonary edema can lead to shortness of breath. While uncommon, pulmonary edema can be life-threatening. A person experiencing edema with shortness of breath should see a doctor right away.
When Dialysis Is An Option
Recent research suggests that people with advanced heart failure who no longer respond well to diuretics may benefit from a procedure called peritoneal dialysis, which can be done at home. A tube called a catheter is inserted into your abdomen, and a sterile cleansing fluid gets pumped in. Its later drained through the tube, carrying excess fluids out with it. One method requires the procedure be done up to five times a day the other method, which is machine-assisted, works overnight as you sleep.
Dont Miss: Heart Rate Is 50 Beats Per Minute
Don’t Miss: Chronic Congestive Heart Failure
How Can I Prevent Heart Failure
You can prevent heart failure by preventing coronary heart disease and heart attack. The best way to do this is to reduce or eliminate the risk factors that lead to heart failure. You could:
- drink alcohol in moderation
- reduce stress and look after your mental wellbeing
If you have had a heart attack, its even more important to manage your risk factors and follow your treatment plan. Make sure you check in frequently with your healthcare team.
Some risk factors such as your age, whether you have other health conditions, or your genes may be outside your control. Speak with your doctor if you have concerns about developing heart failure, and how you can manage it.
Read Also: Heart Rate Sensor
Living Well With Heart Failure
The Heart Foundation has developed a range of resources for people living with heart failure, and their families and carers.
- Living well with heart failure booklet, which includes information about what to do when you feel sick, managing symptoms, and monitoring your fluid and salt intake.
- Living well with heart failure video series, which includes seven videos covering topics to help you manage your condition. The series is available in a range of languages.
- Heart failure fact sheet, which includes questions to ask your health professional and what changes you might need to make to your daily life.
- Heart failure action plan, which helps you to identify the most important parts of your heart failure management to focus on right now.
Access these resources on the Heart Foundation website.
Also Check: Right Sided Heart Failure Vs Left Sided
Fluid Retention: What It Can Mean For Your Heart
Fluid buildup indicates worsening heart failure. Learn how to spot it and treat it early.
The buildup of excess fluid in your body can take a variety of forms from belly bloating and swollen ankles to nausea, persistent coughing and fatigue. You may be tempted initially to dismiss this hodgepodge of problems as having little to do with your heart. However, they all signal water retention, which can mean trouble for people with a history of heart failure.
“Fluid buildup can quickly escalate into a life-threatening situation,” says Dr. Eldrin Lewis, a heart failure specialist at Harvard-affiliated Brigham and Women’s Hospital.
Heart failure may start with injury from a heart attack or develop as a result of damaged valves, infection or disease of the heart muscle cells. Many times, it is the product of years of toil against high blood pressure and clogged arteries. Regardless of what triggers the decline, heart failure culminates in a progressive weakening of your heart’s power to pump.
Consequently, blood circulates through your heart and body more slowly your cells thirst for fresh oxygen and nutrients. To compensate for its weakened state, the heart undergoes a series of structural transformations. Other physical processes also come into play. When the kidneys detect the diminished blood flow, they activate hormones that prompt the body to retain fluid and sodium in an effort to boost the volume of blood in circulation.
